Sleep is vital to human health, but millions of individuals suffer from diseases that disrupt their normal sleep-wake cycle. Two commonly misunderstood but serious neurological disorders are Narcolepsy and Cataplexy. They are connected, but not identical—and an understanding of their similarities, differences, and causes is essential for effective diagnosis and treatment. This article contrasts several disorders from symptoms to remedies, from existing medical knowledge.
Overview of Sleep Disorders: Where Narcolepsy and Cataplexy Fit in
A sleep disturbance is any medical condition that changes the quality, timing, or duration of sleep and disrupts an individual’s daytime functioning. Insomnia, obstructive sleep apnea, restless leg syndrome, and narcolepsy are some of the most common sleep disorders.
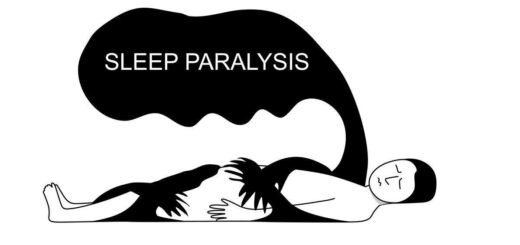
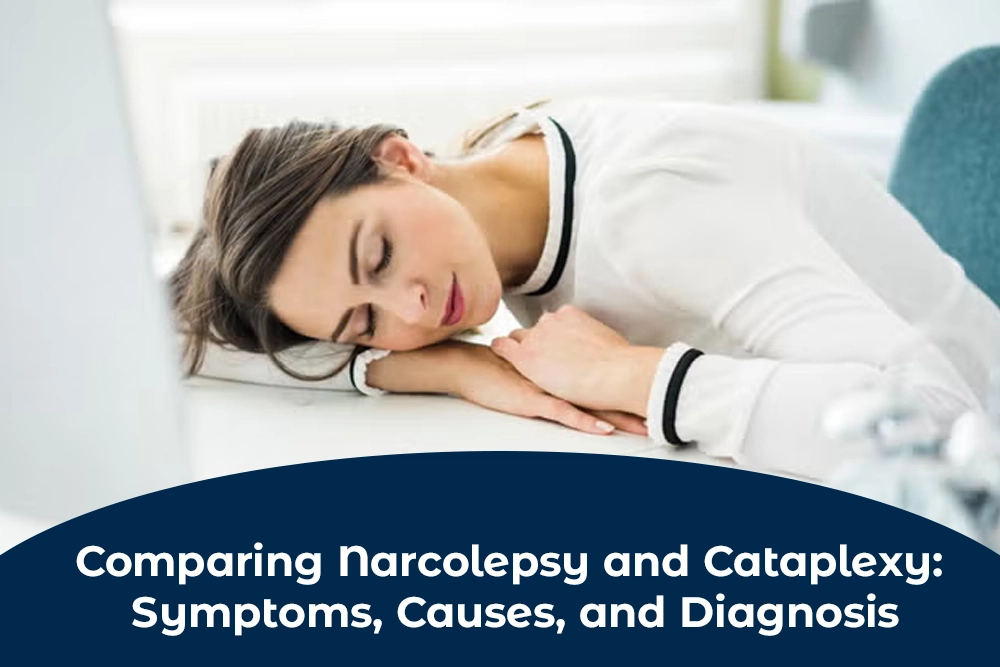
Narcolepsy is a long-term brain problem that makes it hard for the brain to control when you sleep and when you wake up. Those who have narcolepsy often feel sleepy during the day and can fall asleep at any time while doing normal things. Cataplexy, however, is a sudden and brief loss of voluntary muscular tone due to strong emotions such as laughing, anger, or surprise. Although cataplexy is a defining feature of type 1 narcolepsy, it is also considered an independent manifestation that should be given particular consideration in the diagnosis and management.
Knowing where Narcolepsy and Cataplexy fall within the overall spectrum of sleep disorders is essential for reducing misdiagnosis and enhancing patient outcomes.
Real-Life Scenarios: Identifying Symptoms in Everyday Life
To observe how these variables impact everyday life, review these real-world scenarios:
Olivia Scott
Even after a good night’s rest, I find it difficult to remain awake in class. I am beginning to experience “sleep attacks” in the office and during meetings. At times, while laughing excessively, her knees give way and she cannot control her muscles. The association of excessive daytime sleepiness and weakness of muscles may suggest Narcolepsy or Cataplexy.
Emily Parker,
A college student laments of extreme hallucinations upon falling asleep, as well as sleep paralysis. Even though he has never fainted from feelings, his perpetual fatigue and disrupted nocturnal sleep are indicative of narcolepsy without cataplexy, commonly referred to as Type 2 Narcolepsy.
It is vital in both instances to learn to discern the slight distinctions between cataplexy and narcolepsy without. Cataplexy doesn’t affect all persons with narcolepsy, and therefore early indicators might be attributed to laziness, sadness, or other disease. Knowledge and awareness of the actual world clues facilitate efficient disease identification and care.
Neurological causes: What science says about these conditions
Both narcolepsy and cataplexy are brain diseases, but they arise from specific, identifiable changes in brain chemistry and structure.
Narcolepsy, especially Type 1 Narcolepsy, is strongly associated with the loss of neurons that make hypocretin in the hypothalamus. Hypocretin (also referred to as orexin) is a neurotransmitter responsible for controlling arousal, alertness, and appetite. When these neurons are killed—usually due to an inflammatory reaction—the brain cannot maintain a stable sleep-wake cycle.
Cataplexy is straight away linked with hypocretin deficiency. The sudden muscle weakness occurs when the brain inappropriately triggers elements of REM sleep (where muscle atonia normally exists) during wakefulness following strong emotional reactions.
Other elements involved are:
Genetics: Individuals with certain HLA gene mutations are especially susceptible.
Autoimmune dysfunction happens when the body attacks its own nerves by accident.
Environmental triggers: Infections or traumatic events could lead to onset in susceptible persons.
Although the two conditions are triggered by the same neurotransmitter imbalance, cataplexy is a symptom of a more intricate sleep disorder.
Steps Experts Take to Distinguish Between Narcolepsy and Cataplexy
Diagnosis of Narcolepsy and Cataplexy may be complicated by similar symptoms and vagueness of initial warning signs. To confirm the correct diagnosis, sleep experts follow a multi-step approach.
Most Important Diagnostic Steps:
Sleep History and Symptom Questionnaire: Patients are requested to document their sleep habits, number of sleep attacks, emotional precipitants for muscle weakness, and hallucinations or sleep paralysis.
Polysomnography is a test that records your brain waves, oxygen levels, heart rate, and eye movements while you sleep.
Multiple Sleep Latency Test (MSLT): The test, conducted the day after PSG, identifies how rapidly a subject sleeps in a quiet environment during the daytime and whether he or she goes into REM sleep too rapidly (within 15 minutes). This is typical of narcolepsy.
Cerebrospinal Fluid (CSF) Analysis: In certain situations, hypocretin levels are assessed via a lumbar puncture. Low levels very likely indicate type 1 narcolepsy with cataplexy.
Cataplexy is identified by experts based on patient history instead of direct test work since its attacks are unexpectant and transitory. Cataplexy is detectable by looking for overt emotional provocation and the retention of consciousness throughout the episodes.
Tests, Drugs, and Long-Term Treatment Plans
Treating Narcolepsy and Cataplexy requires multimodal therapy incorporating lifestyle modifications, medication, and monitoring. Although a cure doesn’t exist, effective means are available for symptomatic management and enhancing quality of life.
Medications:
Modafinil and Armodafinil are both recommended to treat being too sleepy during the day.
Sodium Oxybate (Xyrem) is used to treat daytime sleepiness and bouts of cataplexy.
Antidepressants, more specifically SSRIs and SNRIs, might reduce the number of cataplexy occurrences by suppressing REM sleep.
Lifestyle changes involve regular daytime naps.
- Regular nighttime habits
- Abstaining from alcohol and large meals at night.
- Employing safety precautions, like refraining from driving in case of frequent sleep attacks.
Long-term treatment of patients suffering from sleep disorders, like narcolepsy, involves routine drug evaluation and dosage adjustments. Cognitive behavioral therapy (CBT) can also help patients cope with emotional and psychological problems related to their disease.
Support Resources: Finding Assistance for Patients and Caregivers
Experiencing narcolepsy and cataplexy may be isolating, but assistance can be had. There are organizations, groups that advocate, and websites with communities offering support, information, and a setting for sharing experience.
Suggested Support Groups:
- Narcolepsy Network.
- Wake Up, Narcolepsy
- National Sleep Foundation
These websites provide educational materials, match patients with physicians, and provide peer support to individuals and families afflicted with a sleeping disorder.
Caregivers should likewise consult and get educated so that they may also know the condition and prevent burnout for their loved ones.
To learn more, visit enquirypharmacy, a trusted resource for health information and treatment options.
Conclusion
Recognition of the connection and contrast between narcolepsy and cataplexy is necessary for proper diagnosis, treatment, and care. Though both conditions result from the same brain abnormality, each manifests differently and impacts daily activities differently. Persons with different sleeping disorders can be living full active lives with speedy diagnosis, suitable medication, and continued care.
The initial step is education and awareness. As a patient, caregiver, or healthcare provider, being more aware of these disorders can eradicate stigma and enhance long-term outcomes.